DYSLIPIDAEMIA
Please forgive me for giving you such a dreadful word – it means undesirable changes in your blood fats. This is a complicated field and I am going to greatly oversimplify it. Please don’t quote any of this back to a lipid specialist or, if you do, say you found it in Readers’ Digest.
Cholesterol and lipoproteins
There are a number of different forms of fat in the blood stream and the form which you will have heard most about is cholesterol. Cholesterol is an important component of cell walls – we all need it if we are to function properly. The cholesterol in the blood is carried by proteins called lipoproteins and can be very roughly divided into two forms – Low Density Lipoprotein Cholesterol (LDL-C) and High Density Lipoprotein Cholesterol (HDL-C).
LDL-C is available for laying down in the walls of the arteries in the plaques of atheroma – the pinch-points which narrow the artery sometimes called “hardening of the artery”. This is “bad” cholesterol.
HDL-C is being carried to the liver where it is broken down and excreted in the bile. This is “good” cholesterol.
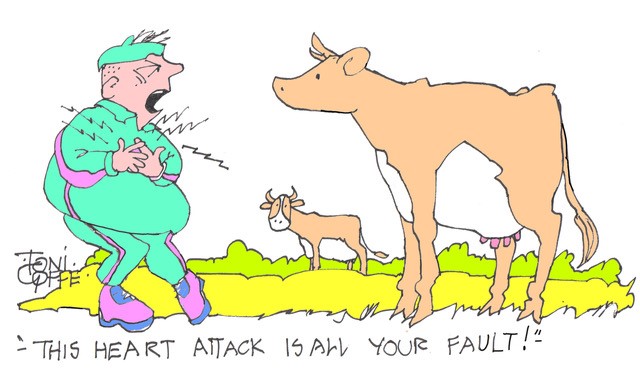
A high level of LDL-C is a risk factor for atheroma – leading to heart attacks and strokes. There is a variety of causes of a high LDL-C including genetic factors, being overweight, having an under active thyroid gland, some forms of kidney disease and eating a high fat diet, particularly a diet with much “saturated” fat. Saturated fat is largely derived from animals – cream, butter, fatty joints of meat and particularly prepared meat products such as meat pies, patés and sausages. Fat is cheaper than lean meat so food manufacturers use it liberally.
A high level of HDL-C protects against atheroma. The main causes of a low HDL-C are diabetes and physical inactivity. The most effective ways of increasing this fat fraction are regular vigorous exercise and losing weight.
Normal and abnormal levels
The “normal” levels of these fat fractions are somewhat arbitrary and there is a tendency for each new generation of cholesterol police to set the limits for total cholesterol and LDL-C lower and lower. Currently the recommended upper limit for total cholesterol is 5.0 mmol/litre and for LDL-C is 3.0. The bell shaped curve of normal distribution would put most of the population in the too-high category.
HDL-C makes up around one quarter of the total cholesterol – the current recommendation is that it should be above 1.0 mmol/l.
A better measure of risk for atheroma and cardiovascular disease is the ratio between total cholesterol and HDL-C. This should be below 4.0 and preferably much lower. This is the measure of cholesterol level used in algorithms for calculating risk of cardiovascular disease – mainly heart attacks and strokes. You can calculate your own risk by visiting www.qrisk.org and filling in information about yourself to give your Q-Risk. Don’t worry if you don’t know all the answers. The algorithm fills in average figures for these.
The medical ill effects of dyslipidaemia
This is all about disease of the arterial system – atheroma, “hardening of the arteries”. Both a high total cholesterol and a high ratio of total cholesterol to HDL cholesterol are powerful risk factors for heart attacks, strokes and peripheral vascular disease (mainly involving the blood supply to the legs). For this reason the total cholesterol/HDL-C ratio is an important element of the Q-Risk assessment for predicting cardiovascular disease. Dyslipidaemia is also a feature of the “metabolic syndrome” which is a combination of obesity, hypertension, diabetes and lipid abnormalities. The metabolic syndrome carries a high risk of atheroma, particularly heart disease.
Treatment of dyslipidaemia
The treatment of dyslipidaemia should involve changes in diet but in practice most people find it very difficult to change the way they eat and maintain new patterns of diet. The modern treatment is the group of drugs known as the statins – and very effective they are too. Not only do they reduce LDL-C by up to 30% and reduce the cholesterol/HDL ratio, they also reduce the risk of atheroma substantially – so substantially that it is regarded as obligatory to prescribe them to all those deemed to be at high risk and particularly to those who already have evidence of arterial disease.
Effect of exercise on lipids
Here I fear I am leading you into choppy seas – the answer to just what effect exercise has on the different fat fractions found in the blood is very unclear.
Prevention
There are age related changes in total cholesterol and LDL Cholesterol – both increasing gradually with time. A study of physical fitness in 11,400 people who had several treadmill tests over 36 years found those in the lower third for fitness developed abnormal lipids 10 to 15 years earlier that those in the fittest third. In other words it does seem that regular exercise delays the age-related development of undesirable changes in blood fats. This idea is supported by the finding that regular walking reduces the both total cholesterol and the all-important ratio of total cholesterol to HDL-C.
Treatment
The data on the response of lipid abnormalities to exercise alone are surprisingly and disappointingly sparse and sometimes contradictory. A 2005 meta-analysis concluded that regular aerobic exercise does raise HDL-C levels but that the effect on other lipid fractions was less certain. It also seemed that exercise alone was less effective than the combination of diet and exercise. However, a 2011 meta-analysis confusingly found that diet and exercise reduce total cholesterol, total cholesterol/HDL-C ratio and LDL-C but has little effect on the protective HDL-C. So, a bit of disparity there but all are agreed that regular exercise does reduce the all-important total cholesterol/HDL-C ratio.
Perhaps the most effective management of dyslipidaemia is the combination of statins with exercise. In a cohort of 10,043 Americans with dyslipidaemia, among men treated with statins the most fit had just 30% the risk of dying over ten years compared with the least fit.
Finally, take heed of the conclusions of the American Heart Association and the American College of Cardiology. After a thorough appraisal of all the evidence they concluded that it may require 12 MET task hours per week of exercise to favourably influence LDL-C. How much is that? – about one hour 40 mins per week of very brisk walking (4 mph). Get to it!
PS
Covid and exercise.
A sobering paper this week from the Transylvanian Review (yes, really). A group of South Korean students who exercised regularly was studied before and after the Covid Lockdown. Over the three months, muscle mass had reduced by 2.2%, while body weight had increased (1.2%), as had fat mass (7.2%) and percentage body fat (9.2%). Cardiopulmonary fitness had reduced by 11% and strength by 5%.
Subscribe to the blog
Categories
- Accelerometer
- Alzheimer's disease
- Blood pressure
- BMI
- Cancer
- Complications
- Coronary disease
- Cycling
- Dementia
- Diabetes
- Events
- Evidence
- Exercise promotion
- Frailty
- Healthspan
- Hearty News
- Hypertension
- Ill effects
- Infections
- Lifespan
- Lipids
- Lung disease
- Mental health
- Mental health
- Muscles
- Obesity
- Osteoporosis
- Oxygen uptake
- Parkinson's Disease
- Physical activity
- Physical fitness
- Pregnancy
- Running
- Sedentary behaviour
- Strength training
- Stroke
- Uncategorized
- Walking


Another superb article by a brilliant cardiologist. One suggestion, nothing to do with the article itself, would be to make the text a bit darker. Aging eyes need greater contrast. Writing this comment in a light grey text against a light gray background is irritating my eyeballs.
Thanks Charlie and sorry about the difficulty reading the Blog
I am trying various ways to improve the contrast and I hope that this week’s posting will be more legible -let me know. Hugh
Helpful and clear. Thank you.