ENCOURAGING EXERCISE Part 2
Adults
In adult life the main bar to exercise is the lack of time resulting from gainful employment and/or bringing up the kids. For you, the working person/parent, the most important incentive to exercise must be an understanding of just how vital this is to your future health, happiness and longevity. If you have not cottoned on to that by now you have not been concentrating – start again and read my Blog more thoroughly!
Medical advice
Encouraging people to take more exercise is a difficult task. Healthcare professionals can, but usually don’t, target appropriate patients. Advice during the consultation is seldom given. A US study of consultations for diabetes or hypertension showed that exercise was recommended on only one sixth of occasions. Even when advice is given it is largely ineffective. A recent meta-analysis of trials of physical activity promotion in primary care did find a slight increase in self-reported physical activity at 12 months but those trials which also measured physical fitness showed no significant increase.
Exercise on prescription
There are many schemes which encourage GPs to prescribe exercise and most local authorities have systems for “exercise on prescription”. The idea is that the GP “prescribes” a course of exercise at the local Sports Centre. The individual has an initial assessment followed by a course of the exercise of around ten weeks at a cost somewhat lower than that charged to the general public. At the end of the course, the individual is encouraged to continue to attend the Sports Centre at the usual rate.
Exercise training and physical activity are not part of the usual medical student’s curriculum and this may explain why the level of referral to such schemes is extremely low. The uptake and completion of prescribed exercise programmes are even lower. Analysis of a number of these schemes shows that such referral systems do not increase physical fitness, health-related quality of life, or exercise habits in the longer term. The idea of exercise on prescription sounds great but more attention needs to be paid to barriers to attendance and continued adherence. Some of the factors which have been identified are a poor organisation of the scheme, inconvenient opening hours, poor social support, and exercise leaders lacking motivational skills.
“Selling” exercise
Exercise schemes can have some effect but only if combined with a lot of extra input to encourage the individual and nurture the changed attitudes and behaviour which are required. A New Zealand study enrolled 1089 women aged 40–74 into a controlled trial of exercise referral and achieved a modest increase in exercising rate in the treated groups at two years. The intervention included initial motivational interviewing, regular follow-up telephone calls (a total of 75 minutes per patient), and a home visit at six months. Even with this level of input, the apparent increased exercise was not associated with improved clinical outcomes but unfortunately was associated with an increased risk of falls and injuries.
The QOF scheme
Prescribing exercise is not part of the thinking of most general practitioners. They have quite enough on their plates and there is no reward for sending the patient to a sporting facility. This is unlike the situation for many aspects of preventive medicine in general practice.
The system called the Quality and Outcomes Framework (QOF) decides a good proportion of the GP’s income. The GP is rewarded for including patients on the obesity register, for getting their blood pressure or blood sugar to an acceptable level, and for prescribing a number of drugs which the NHS recommends. Payment is also made for referral to various agencies for support and education. However, among hundreds of indicators, there is only one related to exercise and that is the number of patients with COPD referred to pulmonary rehabilitation. Otherwise, there is no incentive at all for screening for physical activity or for encouraging physical activity.
Perhaps if a referral to an exercise programme were included in the QOF we might see a benefit for both the individual and the nation as a whole?
Exercise is medicine
Encouraging the population to take exercise needs the commitment of doctors, who should regard exercise as a medicine, as effective a weapon against disease as any drug. The time may be coming for the lifestyle approach. As the BMJ put it “Is lifestyle medicine emerging as a new medical specialty?” The British Society of Lifestyle Medicine was founded in 2016 and this approach is now being adopted by some medical schools, including Cambridge University. Ideally, lifestyle medicine should not need a label of its own but will become integral to the delivery of health care. In its delivery, the medical profession needs to be backed up by political action to make physical activity promotion and facilitation key goals in their public health strategy.
PS
In the post about Yoga a few weeks ago I failed to give you a clickable link to the relevant website. It is well worth a visit and here it is:
Subscribe to the blog
Categories
- Accelerometer
- Alzheimer's disease
- Blood pressure
- BMI
- Cancer
- Complications
- Coronary disease
- Cycling
- Dementia
- Diabetes
- Events
- Evidence
- Exercise promotion
- Frailty
- Healthspan
- Hearty News
- Hypertension
- Ill effects
- Infections
- Lifespan
- Lipids
- Lung disease
- Mental health
- Mental health
- Muscles
- Obesity
- Osteoporosis
- Oxygen uptake
- Parkinson's Disease
- Physical activity
- Physical fitness
- Pregnancy
- Running
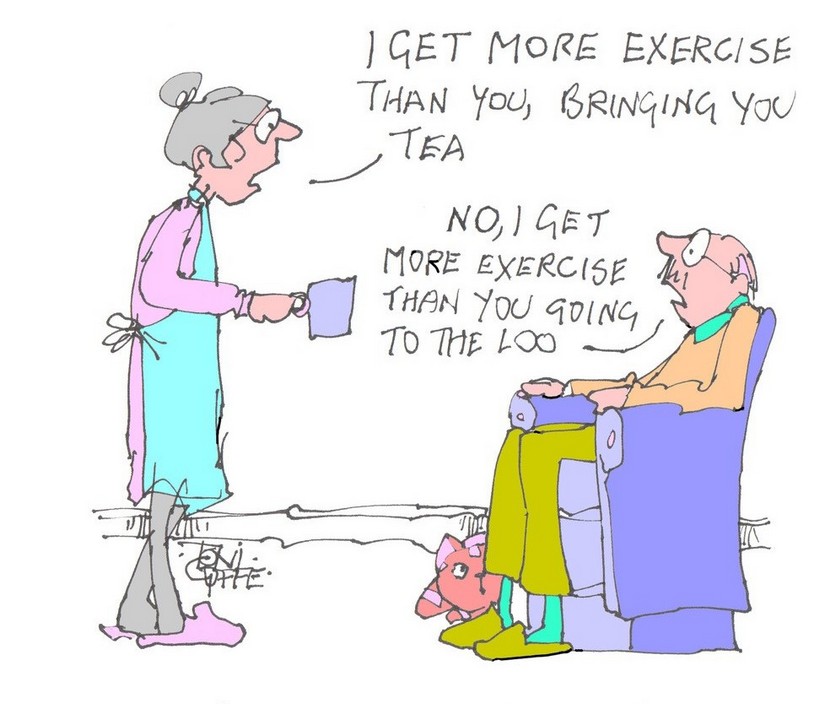
- Sedentary behaviour
- Strength training
- Stroke
- Uncategorized
- Walking


is there any proof that exercise can delay the onset of vascular dementia by improved circulation to the brain?
There certainly is Jenny. Regular exercise and high levels of physical fitness reduce most of the risk factors for cerebral artery disease such as high blood pressure, obesity, diabetes and unhealthy blood fat levels. One study found that compared with inactive people, those who take light exercise roughly halve their risk of dementia in the long term and those who take moderate exercise reduce the risk by two thirds. The benefits seem to include reduced risk of Alzheimer’s disease as well as vascular dementia, though there is some evidence that the effect is greater in preventing vascular dementia – as would be expected.
Always wondered why doctors seemed so slow to recommend exercise and so slow to tell obese people that they are obese and what to do about it. My wife and I apart I am amazed how many are admitting tp putting on weight during lockdown.
Thanks William.
If you wondered why your GP looks more at the computer screen than at you, now you know!
About half the population has gained weight during the lockdowns with an average weight gain of about 3kg. More snacking, more alcohol and less exercise are the main contributors.