FRAILTY PART 4
Healthspan
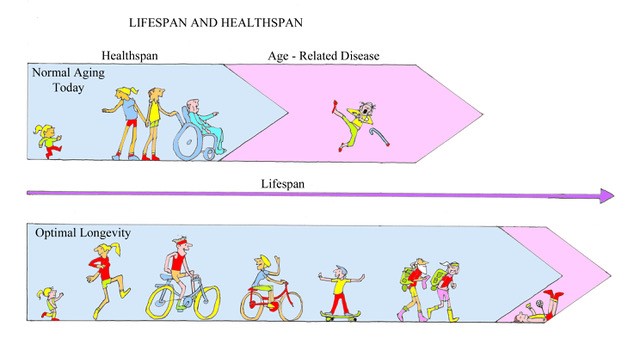
The desirability of decreasing the period of dependency at the end of life cannot be overstated. We are living longer but as our lives extend so also do the years of end-of-life illness and dependency. These are the characteristic of frailty. We should strive for not only more years of life but also for more years of healthy and active life, sometimes referred to as “healthspan”. Healthspan is a much better measure of the health of the nation than lifespan. Shortening the proportion of our lives spent in end-of-life debility is called “compression of morbidity”. This is what we need – to live well until as near to death as possible.
Healthspan versus Lifespan
This week’s illustration above is a representation of Healthspan and Lifespan in two situations. The upper panel depicts our present predicament – our life is long but too much of it spent with disease and disability – the bit at the end after Healthspan. The second panel shows the ideal situation with life being a bit longer but Healthspan much longer so that the period of end-of-life debility is shortened. The upper panel is the outcome of a sedentary life and the lower is the result of a life of physical activity.
The current situation:
Unfortunately the most recent evidence indicates that far from improving, our lives are worsening in this respect. The Office of National Statistics report in 2012 showed that a 65-year-old man could expect to be free from disability and long-term illness for a further 10.6 years but by 2014 this had decreased to 10.3 years. For women, the figures were 11.2 years falling to 10.9 years. Oh dear.
Another way of looking at it is the life expectancy of someone born today. A boy born now can expect to live to the age of 78.5 but only have a healthy life expectancy (healthspan) of 62.7. ie 20% of his life will be with some form of disability or chronic illness. The picture for women is even worse – life expectancy 82.5 years, healthy life expectancy 63.9 giving a total of 23% of life expectancy being lived with a chronic illness or disability. No wonder we have such a growing social care crisis.
Exercise for prevention of frailty
End-of-life frailty and dependency is mainly the long-term result of an accumulation of one or more of the degenerative diseases which I have described previously – the non-communicable diseases. They are all promoted by lack of exercise. The main risk factor for the development of frailty is insufficient physical activity – over a very long period. The idle and the sedentary are those at risk – and the risk is very much allied to physical fitness.
The influence of physical fitness
Physical fitness is a product of a number of factors including age, hormonal changes, heredity, socioeconomic status, etc, but only one risk factor is easily influenced by the individual – the level of physical activity. A study of non-elite cyclists aged 55 to 79 found very high levels of fitness. For those aged 55 the fitness was equivalent to the average for 20-year-olds, for those aged 65 it was equivalent to the average for 25-year-olds and for those aged 75 it was equivalent to 35-year-olds!
Similar findings were found by the Stanford Arthritis Centre study of runners aged over 50 compared with non-exercising controls. Over 500 members were followed up over nine years and compared to a similar number of non-running members of the same community. The disability scores were low in both groups at the start of the study and remained so in the runners over the whole period of follow-up. However, the disability scores in the non-runners rose steadily throughout the nine years. When this group was followed up for a total of 19 years the benefits sustained by the runners continued to accumulate. The average time until the onset of measurable disability was 16 years later for the runners compared with the controls. The health gap between the groups increased through the period of study and was still widening into the tenth decade of life.
The improved health status of elderly people who have exercised regularly has been emphasised by one study which found that the average 65-year-old can expect an additional 12.7 years of healthy life – meaning that he will live disability-free until age 77.7. Highly active 65-years-olds, however, have an additional 5.7 years of healthy life expectancy – they will remain disability-free until age 83.4.
Exercise in the treatment of frailty
Although some improvements in function may result from exercise interventions to treat the elderly infirm, once frailty has set in it may be too late to make major differences to performance.
A 2008 meta-analysis of exercise interventions showed improvements in both functional and physical performance in the treated groups but no increase in ability to perform activities of daily living (ADLs). A further review in 2011 confirmed a limited benefit from applying exercise programmes to frail older adults and found that only more prolonged and vigorous exercise programmes were effective in improving functional ability – “multicomponent training interventions, of long duration (≥5 months), performed three times per week, for 30-45 minutes per session, generally had superior outcomes than other exercise programs”.
However, for elderly patients who already have some functional limitations, further decline in physical functioning can be slowed by maintaining even a low level of physical activity. The LIFE study in the US randomised a volunteer sample of 1635 mildly impaired sedentary men and women aged between 70 and 89 years into a programme of physical training or no intervention. The treated group showed significantly better mobility in the treated group after 2.6 years of training. This effect is seen in “younger” old people and the less disabled but exercise may not help the very disabled particularly those with severely limited mobility – exercise intervention is needed before debility has gone too far.
A trial that investigated weight-training in nursing home residents, aged 90 years or older, showed the training to be clearly beneficial in terms of strength and self-care scores – but the scores soon fell back to their pre-trial levels after the study ended.
Poor balance and falls
A particular role for exercise as a treatment for frailty is in the prevention of falls in those who have already suffered accidental tumbles. Around one-third of over 65s and half of over 80s fall at least once a year. Falls are the leading cause of death from injury in the over 70s. Falls lead to fractures including 80,000 hip fractures per annum in the UK. The provision of exercise and education programmes to reduce the risk of falling is growing, an example being those set up by ambulance stations for the patients who they have helped pick up from the floor. A large meta-analysis of such programmes involving more than 4,000 elderly fallers has shown a subsequent reduction in falls by 30% and of falls leading to fractures by 60% – worthwhile indeed
The 2018 Cochrane review of the use of exercise to prevent recurrent falls in the elderly concluded that a combination of balance and functional training with strength training is effective. If widely applied this should reduce by a quarter the overall number of falls per year which would amount to about 140 fewer falls per 1000 older people over one year in the general population and twice as many in older people at high risk of falls.
However, if it is to be any good at all, the exercise must be maintained – something which becomes increasingly difficult for the elderly.
The message is clear – it is never too late to take up exercise but if you leave it too long you may have missed the boat as far as reduction in dependency is concerned. And as you get older it becomes increasingly important to maintain a physically active lifestyle. Lapsing into a lazy old age is a recipe for detraining and the onset of dependency.
Remember to see “How not to kill Granny”. Go to:
https://medium.com/in-fitness-and-in-health/dont-kill-granny-7fe1b5d5a883
Subscribe to the blog
Categories
- Accelerometer
- Alzheimer's disease
- Blood pressure
- BMI
- Cancer
- Complications
- Coronary disease
- Cycling
- Dementia
- Diabetes
- Events
- Evidence
- Exercise promotion
- Frailty
- Healthspan
- Hearty News
- Hypertension
- Ill effects
- Infections
- Lifespan
- Lipids
- Lung disease
- Mental health
- Mental health
- Muscles
- Obesity
- Osteoporosis
- Oxygen uptake
- Parkinson's Disease
- Physical activity
- Physical fitness
- Pregnancy
- Running
- Sedentary behaviour
- Strength training
- Stroke
- Uncategorized
- Walking


I totally agree with the importance of exercise for the elderly. I am 74 and have a shoulder injury (lack of cartilage causing bone on bone) that does not allow me to do upper body strength training. How can I compensate for my lack of limited upper body movement and still gain upper body strength?
Thank you
Thanks Mike and sorry to hear about your shoulder. This may not apply to you, but many shoulder injuries cause pain for a limited time – usually between one and two years. Shoulder joints are non-weight bearing which does allow recovery from injury more readily than applies for weight bearing joints.
I have three thoughts. First, maintain what movement you have as well as you can. Second, compensate by exercising your other arm more. Third, try Charles Atlas-type exercises. That involves holding the affected arm still with the good side and pushing against it in the five directions of shoulder mobility – flexion (pushing forward), extension (pushing backwards), abduction (pushing outwards), internal rotation (with the elbow bent to right angles rotate the forearm across the chest) and external rotation (rotate the forearm the other way, away from the body). The idea with each of these movements is that you tense the muscle which would have created the movement but the shoulder does not move at all. The muscular effort helps to maintain or improve the muscle’s strength. Try doing each exercise to the count of ten and repeat five times or until bored!
I hope that this helps