MORE ABOUT EVIDENCE
We are repeatedly reminded by politicians that their decisions are dictated by “the science” which is often shorthand for “this is how we have used science to justify what we are about to do”. As John Barry said “When you mix politics and science, you get politics.”
I hope that one thing you might have begun to suspect from last week’s blog is that “the science” is very inexact. It would be best to call it “the interpretation of chosen scientific facts”.
Interpretation
Medicine is very far from being a perfect science – it is said that half of what doctors believe to be true today will, in time, be shown to be wrong. The trouble is that we do not know which half. Interpreting evidence is a huge problem but it is at the heart of “evidence based medicine”.
It is important to make medicine as scientific as possible and to question the validity of the evidence we use to that end. The gold standard for testing the accuracy of a belief in the effectiveness of a treatment is the randomised controlled trial (RCT) which I described in last week’s Blog. The credibility of evidence can be stratified into levels. The highest level is provided by systematic reviews and meta-analyses (see last week’s Blog) of all relevant randomised controlled trials (RCT’s). The lowest level is the opinion of authorities and/or reports of expert committees.
In the following Blogs I will not be giving a full review of all the evidence for each statement on the effects of exercise. That would not make exciting reading. But I will include some of the more important or convincing research. In particular I will be referring frequently to “Cochrane Reports”. The Cochrane Collaboration is an independent non-profit making group which conducts systematic reviews and meta-analyses of RCTs of health care interventions across all aspects of medical treatments. If you need or wish to check on the evidence for any particular treatment, just Google Cochrane and enter their website for the most comprehensive assessment of evidence based interventions or drugs in the world.
Presentation of Evidence
It is very easy to be misled by the way in which that evidence is presented. Those with an axe to grind, including those funding the study, are likely to present their results in a way which is most likely to persuade the reader that the treatment is effective. This is well demonstrated by the fact that trials and meta-analyses funded by drug companies are far more likely to favour the drug in question than those receiving independent funding. Be warned too that negative studies are much less likely to reach the light of day than those with positive findings. The failure to publish negative trials is a particular problem for meta-analyses.
Fortunately exercise studies are seldom sponsored by commercial organisations but nevertheless the authors of studies do sometimes have an interest in the outcomes – be aware of this possible bias.
One more point on the presentation of evidence. The benefit of a particular intervention is usually expressed in terms of change in risk which may be presented as a change in relative risk or a change in absolute risk. The change in relative risk usually makes the treatment seem much more attractive than the change in absolute risk.
Absolute versus relative risk
Absolute risk of a disease is the risk of developing the disease over a time period and may be expressed as a ratio, a percentage or as a decimal. If you have a one in five risk (ratio) of developing a disease this may be expressed as a 20% risk (percentage) or as 0.2 (decimal).
*Relative risk is used to compare the risk in two different groups of people. For example, the groups could be smokers and non-smokers. All sorts of groups are compared to others in medical research to see if belonging to a particular group increases or decreases your risk of developing certain diseases (see my previous Blog about epidemiology) For example, research has shown that smokers have a higher risk of developing heart disease compared to (relative to) non-smokers.
Let us say that the absolute risk of developing heart disease is 4 in 100 (4%) in non-smokers but the relative risk of the disease is increased by 50% in smokers. The 50% relates to the 4 – so the absolute increase in the risk is 50% of 4, which is 2. So, the absolute risk of smokers developing this disease is 6 in 100. If the two groups are compared, the increase in risk brought about by smoking is 2 in 100 – for every 100 smokers, 2 more individuals will develop heart disease compared to non-smokers.
When comparing the results of treatments, whether the outcomes are expressed as absolute or relative improvements can have a big effect on how good the treatment looks. The less common the condition the more this is so. Take the example of the risk of a heart attack and how this can be reduced by taking a particular drug. The risk of a heart attack over the next ten years in a group of women aged between 40 and 50 may be, say, one in a hundred – 1%. If taking the drug in question reduces the risk to one in 200 (0.5%) it may be reported that the risk of a heart attack, the relative risk, was halved in this group. This sounds a pretty good effect. However the absolute risk is a reduction from two deaths to one death for every 200 women – an absolute reduction of one in 200. In other words, 200 women would have to take the drug for ten years to prevent one new heart attack – which seems rather less impressive than halving the risk. Sometimes the effectiveness of a treatment is then expressed as number needed to treat, the number of people who need to take the treatment for just one person to benefit – in this case 200.
Mortality
Mortality rates are often used as outcome measures to compare the efficacy of different drugs and other treatments. Since the ultimate mortality for any management system is 100% – we all die in the end – “mortality” when used for this end has to be qualified. There are two ways of doing this:
1. Mortality is expressed as the death rate over the period of study and compared between the groups being studied.
2. The death rate of a group under study is compared with the known death rate of the whole population of the same age and gender – it is usually expressed as deaths per 1,000 persons per year.
PS
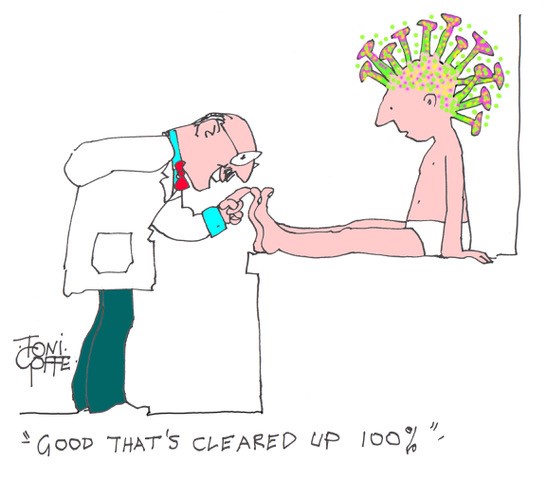
Covid again. Every day we are bombarded with more and more facts about the virus and its effects on people, society and our physical, mental and financial health. Often the information is slanted by the interests of those reporting to us – viz the Telegraph versus the Guardian.
May I recommend the fortnightly reports in Private Eye, written by “MD” who is the well known medical journalist, Dr Phil Hammond? His reports are admirably concise and easy to read and not afraid to expose some of the mishandling and the misinformation which has been dished out to us from other sources. In this week’s report he reinforces my recommendation for a healthier lifestyle as a powerful way to reduce your risk of dying from Covid-19 (or a long list of other avoidable diseases). He regrets that the government has missed “a golden opportunity to improve public health while it had the nation’s full attention……….Matt Hancock serving salad and sleep tips in a leotard would have been far more use than his vacuous and inaccurate press briefings.”
Taking regular exercise may have an important part to play in increasing your ability to withstand the ravages of the virus if you are unlucky enough to catch it. So keep it up…….
Subscribe to the blog
Categories
- Accelerometer
- Alzheimer's disease
- Blood pressure
- BMI
- Cancer
- Complications
- Coronary disease
- Cycling
- Dementia
- Diabetes
- Events
- Evidence
- Exercise promotion
- Frailty
- Healthspan
- Hearty News
- Hypertension
- Ill effects
- Infections
- Lifespan
- Lipids
- Lung disease
- Mental health
- Mental health
- Muscles
- Obesity
- Osteoporosis
- Oxygen uptake
- Parkinson's Disease
- Physical activity
- Physical fitness
- Pregnancy
- Running
- Sedentary behaviour
- Strength training
- Stroke
- Uncategorized
- Walking