Obesity Part 3.
The causes of obesity
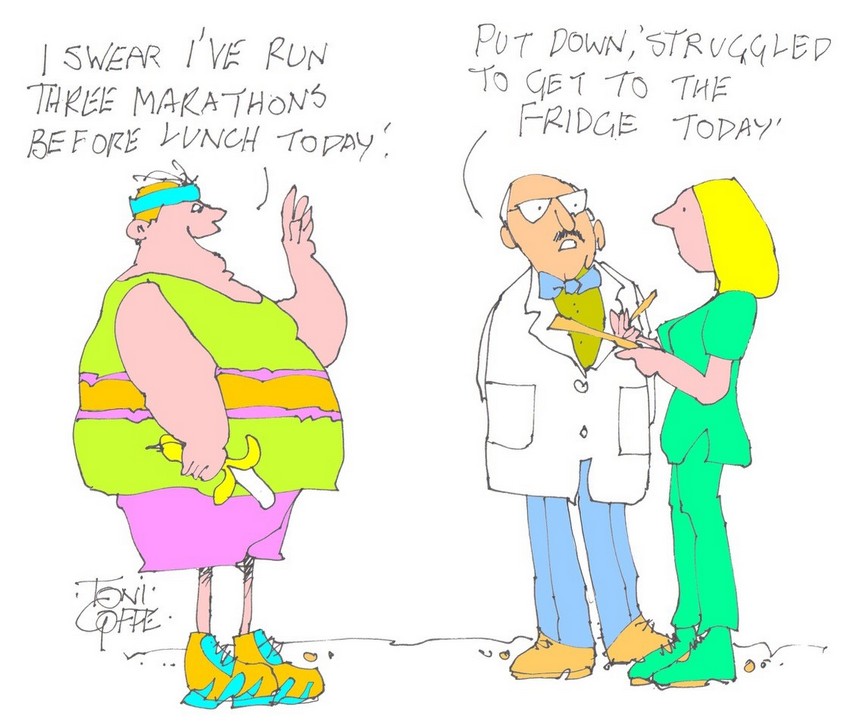
In my last Blog I briefly discussed genetics and diet as causes of obesity – but had no space for exercise. So:
Exercise:
Change in body weight is decided by the balance between calories in (what you eat) and calories out (how much you move about). There are any number of other factors which can contribute to either of these sides of the equation such as inherited characteristics, sleeping patterns, drugs, socio-economic status, ethnicity, psychological stress etc, etc.
People who have a high level of physical activity from childhood are very rarely obese.
Individuals with obesity in the UK are two to three times more likely to report low levels of physical activity compared with normal-weight adults and have higher rates of sedentary behaviour. The reasons for this are complex, and individuals living with obesity face many barriers to becoming more physically active. These can include feelings of shame, associated multiple health conditions and symptoms, sedentary work and lack of access to green space.
The management of obesity
Losing weight is really, really difficult. So for the management of obesity, prevention is much easier than treatment. By adult life our dietary and exercise habits are well ingrained and changing our lifestyle/daily habits is hard indeed. Losing weight by diet alone is usually more effective than by exercise alone but the combination does carry the best chance of success. This means two aspects of behaviour to change. How hard is that? Actually very hard indeed particularly when the contributory causes I mentioned above are concerned.
Overweight and obesity usually starts in childhood – the key to a healthy, normal weight population must be to start young. Unfortunately the figures for childhood obesity are rising inexorably and this is driven in part by socio-economic deprivation. The more deprived an area, the lower the levels of physical activity and the more people there are living with obesity. This difference starts in childhood. Rates of childhood obesity have risen sharply in recent years, more so in the most deprived areas. In 2020/2021 in England, rates of obesity in poorer areas among 4-year-olds were more than double that of richer areas (6.2% versus 13.6%). The gap was wider still by age 10 (13.5% versus 31.3%) and persists through adulthood (19.2% versus 36.8%). This difference is not inevitable. What has changed since 1993, and what differs between affluent and deprived areas, is not people’s genes or willpower but the proliferation of environmental factors that increase an individual’s likelihood of gaining weight.
The NHS approach:
The NHS has a four tier approach to the management of obesity.
Tier 1 – universal services: This involves diet and physical activity aiming at behavioural change, reinforcing healthy eating and physical activity messages.
Tier 2 – Lifestyle management: A mixture of primary care (GPs, dieticians) including referral to commercial weight loss programmes.
Tier 3 – Specialist weight management: Referral is for those who have failed to lose weight through Tier 1 and Tier 2 interventions. Interventions include low energy liquid diets, further endocrine investigation and assessment for bariatric surgery (stomach bypass)..
Tier 4 – Mainly bariatric surgery: This is one treatment which really does work for obesity. However it does involve a major operation and is only considered for those with either a BMI of 40 or more or those with a BMI between 35 and 40 together with another risk factor such as diabetes or high blood pressure.
Mind you, most of this is wishful thinking. A recent study has found that only about 3% of overweight or obese patients are referred to NHS weight control clinics and even for the morbidly obese (BMI 40kg/m2 or more) the referral rate is less than 10%.
Bariatric surgery:
There are three operations under this heading
- gastric band – a band is placed around your stomach, so you do not need to eat as much to feel full
- gastric bypass – the top part of your stomach is joined to the small intestine, so you feel fuller sooner and do not absorb as many calories from food
- sleeve gastrectomy – some of your stomach is removed, so you cannot eat as much as you could before and you’ll feel full sooner.
Weight loss surgery can achieve dramatic weight loss, but it’s not a cure for obesity on its own.
You’ll need to commit to making permanent lifestyle changes after surgery to avoid putting weight back on. This involves both dietary changes and maintaining as high a level of physical activity as possible
Medication
When all else fails, try reading the instructions – or try medication! See “Obesity Part 1 – drug treatment” the Blog from 23rd Sept.
Next time
Next time some final thoughts about this thorny topic before moving onto some recent research results.
Subscribe to the blog
Categories
- Accelerometer
- Alzheimer's disease
- Blood pressure
- BMI
- Cancer
- Complications
- Coronary disease
- Cycling
- Dementia
- Diabetes
- Events
- Evidence
- Exercise promotion
- Frailty
- Healthspan
- Hearty News
- Hypertension
- Ill effects
- Infections
- Lifespan
- Lipids
- Lung disease
- Mental health
- Mental health
- Muscles
- Obesity
- Osteoporosis
- Oxygen uptake
- Parkinson's Disease
- Physical activity
- Physical fitness
- Running
- Sedentary behaviour
- Strength training
- Stroke
- Uncategorized
- Walking