PERIPHERAL VASCULAR DISEASE
Atheroma and Peripheral Vascular Disease (PVD)
The cause of PVD
Atheroma – popularly known as “hardening of the arteries” – can involve any part of the vascular tree. The most important ill effects of atheroma involve the heart (heart attacks) and brain (strokes). Arterial disease elsewhere is known as peripheral vascular disease (PVD) and the commonest parts affected are the legs. The main risk factors are diabetes, cigarette smoking, high blood pressure, dyslipidaemia and of course lack of exercise. In a minority there is a strong inherited predisposition.
Frequency and symptoms
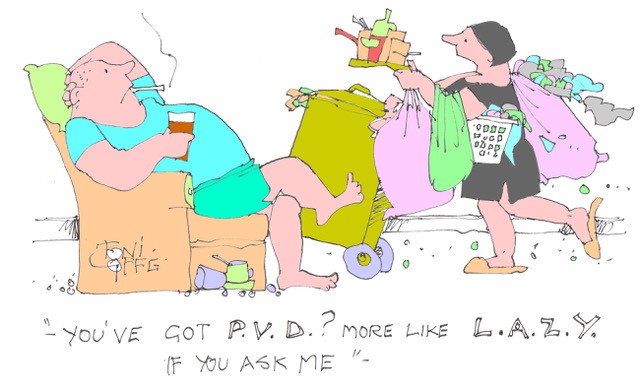
PVD affects roughly 5% of those over the age of 65 years. It is much more common in diabetics of whom the number affected are about 10% by ten years after diagnosis rising to 45% after 20 years. The combination of diabetes and smoking is particularly dangerous. Like coronary disease, PVD initially causes muscle pain on exertion – usually pain in the calf with walking, resolving rapidly on stopping. Just like angina, but of the legs muscles instead of the heart muscle. This is called intermittent claudication – or intermittent limping named after the Roman emperor Claudius, a famous limper.
Progression of the arterial narrowing may lead to complete blockage of an artery resulting in severe lack of blood to the feet. The lower parts of the legs may develop ulcers which won’t heal. Toes become painful, then white and ultimately black and gangrenous, requiring amputation.
Penile blood supply may also be affected by PVD causing erectile dysfunction (ED). Erections are absent, weak or cannot be sustained – a cause of much distress and frustration to those so afflicted. Both low fitness and muscular weakness predict an increased likelihood of ED.
Exercise to prevent PVD:
PVD is closely linked to other forms of arterial disease. About 60% of PVD sufferers have concurrent coronary artery disease and 30% have cerebrovascular disease. Preventive measures for all these diseases are very similar. Regular exercise and high levels of physical fitness reduce three out of the four most important risk factors for PVD – that is to say diabetes, high blood pressure and abnormal blood lipids. Regular exercisers rarely suffer from PVD.
Exercise to treat PVD:
There are operations to restore blood supply – either bypass grafting or angioplasty (as for coronary artery disease but easier because you don’t need to stop the heart) – but these are only needed when symptoms are severe or when the limb is threatened. The only other effective treatment is exercise, particularly walking. The best results are obtained when the sufferer walks for more than 30 minutes on three days per week or more to the greatest degree of calf pain tolerable – and keeps it up for at least six months. Supervised walking is more effective than unsupervised. The Cochrane review of this treatment covered 1837 adults in 32 trials. The treated groups showed significant increases in both pain free walking distance and maximum walking distance.
The way in which walking improves intermittent claudication is probably by provoking muscle ischaemia (inadequate blood supply) which encourages the growth of new small blood vessels (collaterals) to bypass the narrowed or occluded arteries. Structural changes in the walking muscles also contributes.
PS
Sports and disease prevention
A study from Australia has reported on the effects of participating in sports and risk of disease. The findings were that running, tennis, team sports, exercise classes and resistance training were associated with reduced odds of hypertension. Running, cycling, resistance training and yoga/taichi were associated with reduced odds of diabetes. Cycling, tennis, home-based exercises, resistance training and yoga/taichi were associated with lower odds of obesity.
Whichever you choose it is going to do you good…………..
Subscribe to the blog
Categories
- Accelerometer
- Alzheimer's disease
- Blood pressure
- BMI
- Cancer
- Complications
- Coronary disease
- Cycling
- Dementia
- Diabetes
- Events
- Evidence
- Exercise promotion
- Frailty
- Healthspan
- Hearty News
- Hypertension
- Ill effects
- Infections
- Lifespan
- Lipids
- Lung disease
- Mental health
- Mental health
- Muscles
- Obesity
- Osteoporosis
- Oxygen uptake
- Parkinson's Disease
- Physical activity
- Physical fitness
- Pregnancy
- Running
- Sedentary behaviour
- Strength training
- Stroke
- Uncategorized
- Walking


Thank you for that information. I suffer but was advised about exercise and it really improved the pain in my leg.
Delighted to hear it Jean – keep walking! Hugh