THE CONSEQUENCES OF BEING OVERWEIGHT OR OBESE
Is obesity a disease?
There is disagreement in both the medical profession and in the general public about the status of obesity – is it a disease or is it merely the result of unwise lifestyle choices?
1. Obesity as a disease: Certainly obesity satisfies some of the definitions of a disease – and the American Medical Association does define it as such. It is argued that there are a number of external causes such as health inequalities, genetic influences and social factors. Obesity carries serious health risks and if it is defined as a disease it will be treated more seriously and doctors will feel freer to talk to their patients about weight as an important medical issue. Defining obesity as a disease reduces “fat shaming” which often seems to encourage further weight gain. Funding should also be more forthcoming, particularly in countries where medical care is paid from insurance policies.
2. Obesity as a lifestyle choice: It is hard to define obesity consistently. Body Mass Index (BMI) doesn’t apply to everyone, including endurance athletes and weightlifters. Obesity doesn’t always reflect poor health. Obesity can be a risk factor for other medical conditions, but it doesn’t guarantee a person will have health problems. Calling obesity a disease can foster a culture of personal irresponsibility. A disease seems like something which has been imposed from without. How can anyone who believes that they are a victim of uncontrollable outside forces come to understand that they can change their own situation for the better?
A powerful risk factor
Personally I do not agree that obesity is a disease but it is certainly a powerful risk factor for a number of dangerous illnesses which include such age-related conditions as type-2 diabetes, high blood pressure, heart attacks, strokes, oesophageal reflux, painful leg joints and several varieties of cancer (uterus, breast, bowel, gullet, ovary, liver and pancreas for a start). Obesity also contributes significantly to disability in later life making old people less able to carry out normal activities of daily living and more likely to become frail and dependent.
I will consider each of these conditions in turn over the following months.
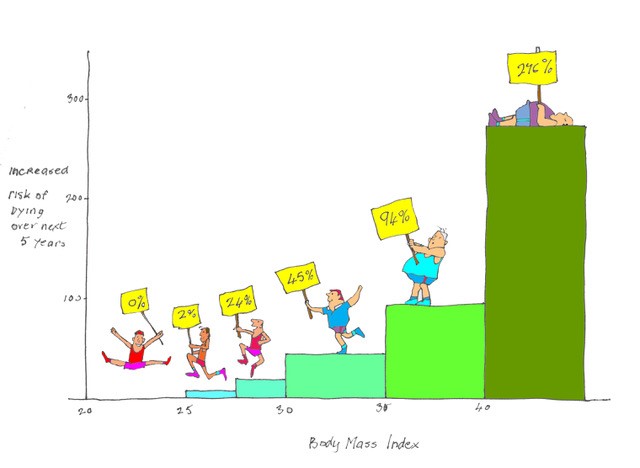
Mortality
With obesity, standardised mortality rate (age-related mortality rate compared with national average) increases by 30% for every increment of 5 above a BMI of 25. A recent study of more than 10.5 million people over four continents has clarified the mortality risk of being overweight or obese. At mild degrees or overweight the increased risk is small but with increasing body mass index (BMI) there is an exponential rise in risk. Compared with those of normal weight (BMI 20-25kg/m2), having a BMI between 25 and 27.5 increases risk of death over the following 5 years by 7%, a BMI of between 27.5 and 30 increases risk by 20%, a BMI between 30 and 35 increases risk by 45%, a BMI between 35 and 40 by 94% and a BMI over 40 increases risk by a staggering 276%. The illustration above illustrates exponential increase in mortality with increasing BMI.
It has been estimated that our obesity epidemic shortens lives by as much as nine years and costs wider society £27bn a year. The risks are much greater for men than for women at all levels of obesity. About one in seven premature deaths in Europe is due to being overweight or obese. Overweight people lose on average one year of life and obese people lose about three years of life.
Can you be too thin?
Maybe – there is a U-shaped curve which describes the relationship between BMI and mortality – the lowest mortality being at about 22. Lower BMIs are associated with increased mortality. It is presumed that thin people include those who are thin because they suffer ill health or have unhealthy behaviours such as smoking.
Other ill effects
Other important ill effects of obesity include:
- Aggravation of breathlessness. Think of carrying a heavy suitcase around all day.
- Worsening of asthma. The weight of the chest wall presses down on the airways.
- Hip. knee and ankle pain. The poor old joints are taking an increased load.
- Sleep apnoea. This potentially dangerous condition is much more common in the obese. Snoring is accompanied by periods of interrupted breathing, waking the subject, sometimes many times during the night. This leads to sleep deprivation and daytime fatigue with a tendency for drivers to fall asleep at the wheel – dangerous indeed. Sleep apnoea is also associated with high blood pressure and coronary disease.
- Poor quality of life. The more you weigh the more difficult it is just to get around. Most fat people have a low cardiorespiratory fitness level and their reduced quality of life often promotes poor mental health, particularly depression.
Next week I will discuss ways in which exercise can be used to manage obesity.
PS
Obese older people are more likely than their slimmer peers to suffer from painful hips, knees and ankles. I have always believed that this is because they are more prone to wear and tear arthritis (osteoarthritis) because of the load they have to carry around. A recent study of body fat and joint disease has indicated that the percentage of body fat is related more to joint and muscle pain than to the severity of the arthritis1. Increasing fat is also related to increasing inflammation and thus more pain. Weight loss for those with lower limb arthritis should therefore bring two pain relieving benefits – less inflammation and less strain on the joints.
- DOI: 10.1002/art.41222
Subscribe to the blog
Categories
- Accelerometer
- Alzheimer's disease
- Blood pressure
- BMI
- Cancer
- Complications
- Coronary disease
- Cycling
- Dementia
- Diabetes
- Events
- Evidence
- Exercise promotion
- Frailty
- Healthspan
- Hearty News
- Hypertension
- Ill effects
- Infections
- Lifespan
- Lipids
- Lung disease
- Mental health
- Mental health
- Muscles
- Obesity
- Osteoporosis
- Oxygen uptake
- Parkinson's Disease
- Physical activity
- Physical fitness
- Pregnancy
- Running
- Sedentary behaviour
- Strength training
- Stroke
- Uncategorized
- Walking


Dear Hugh
I used to work for Weight Watchers and we always said Obesity is not a disease, it is your way of life.
Regards,
Gillian
Thanks Gillian – see next week for more about this
Hugh