The Ill Effects of Obesity.
Non-communicable Diseases
Obesity is not a disease, but it is a powerful risk factor for a number of dangerous illnesses, including such age-related conditions as lower-limb osteoarthritis, type 2 diabetes (T2DM), dementia, hypertension, heart attacks, atrial fibrillation, strokes, oesophageal reflux, fatty liver and several varieties of cancer (uterus, breast, bowel, gullet, ovary, liver and pancreas for a start). These are the Non-Communicable Diseases (NCDs) which are now the chief causes of ill health, frailty and premature death in Westernised societies.
There is an interconnectedness between all these conditions. For instance T2DM is related to an increased risk of hypertension, heart attacks, dementia and strokes. Hypertension carries an increased risk of heart attacks, atrial fibrillation and strokes – and so on. Connecting them all is a lack of exercise and low levels of physical fitness.
Frailty and disability
Both quality of life and productivity are considerably reduced for the obese. Obesity also contributes significantly to disability in later life, making old people less able to carry out normal activities of daily living and more likely to become frail and dependent.
Mortality
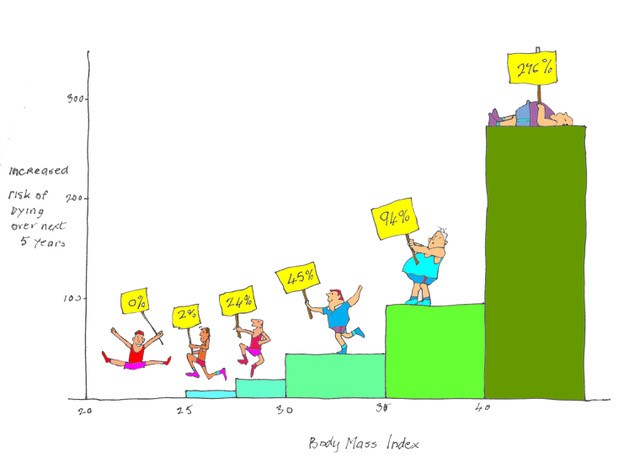
Mortality rate increases by 30 per cent for every increment of 5 above a BMI of 25.Curiously, while 45 per cent of deaths of those with a BMI of 30 or more are due to obesity-related diseases, obesity is seldom recorded as a contributory factor on death certificates.
The histogram which heads this Blog illustrates the increased risk of premature death in obese subjects and comes from a recent study of more than 10.5 million people over four continents. Compared with those of normal weight (BMI 20–25), having a BMI between 25 and 27.5 increases risk of death over the following five years by 7 per cent; a BMI between 27.5 and 30 increases risk by 20 per cent; a BMI between 30 and 35 increases risk by 45 per cent; a BMI between 35 and 40 increases risk by 94 per cent; and a BMI over 40 increases risk by a staggering 276 per cent.
The risks are much greater for men than for women at all levels of obesity. About 1 in 7 premature deaths in Europe is due to being overweight or obese; overweight people lose on average one year of life; and obese people lose about three years of life. However, being thin is not always healthy. BMIs below 22 are also associated with increased mortality. It is presumed that thin people include those who are thin because they suffer ill health or practice unhealthy behaviour such as smoking.
And it is not only the CDMs. The risk of dying from Covid-19 is doubled for obese patients.
Other ill effects
Other important ill effects of obesity include aggravation of breathlessness; worsening of asthma; damage to joints, particularly knees and hips; abnormal blood lipids; depression; and sleep apnoea. Wouldn’t you do anything to avoid that lot? Either the answer is yes or you are not paying attention.
And cost
Obesity is much more than a medical problem. In 2015 in the UK the cost to the NHS directly attributable to obesity was £4.2 billion and the cost to the wider economy was £27 billion. And as we get fatter our perceptions change: the new norm is to be overweight or obese, with the likely knock-on consequence of an increasingly corpulent population.
Subscribe to the blog
Categories
- Accelerometer
- Alzheimer's disease
- Blood pressure
- BMI
- Cancer
- Complications
- Coronary disease
- Cycling
- Dementia
- Diabetes
- Events
- Evidence
- Exercise promotion
- Frailty
- Healthspan
- Hearty News
- Hypertension
- Ill effects
- Infections
- Lifespan
- Lipids
- Lung disease
- Mental health
- Mental health
- Muscles
- Obesity
- Osteoporosis
- Oxygen uptake
- Parkinson's Disease
- Physical activity
- Physical fitness
- Pregnancy
- Running
- Sedentary behaviour
- Strength training
- Stroke
- Uncategorized
- Walking


I couldn’t agree more about keeping one’s weight low and steady. In my 20s I weighed 62kg, now I weigh 59kg but I have shrunk to 1.40m which makes it an unfavourable BMI indeed. I understand there are two schools of thought on scoliosis. One says you take the height you are now, the other says you take the height you once were.
Thanks Numa. It is your original height which is the best indicator.
Hugh,
I do think that GPs should be more honest with their patients and tell them to lose weight. Also tell the parents of small kids who are starting to increase their weight. I know it can be difficult and none of us like to be criticised, but it is such a huge problem and so costly both in health and money.
Thanks Jean.
There is a great debate on so-called “fat shaming” which is levelled at attempts to inform people.. My own view is that your are right but unfortunately telling people that they should lose weight is largely ineffective. But so is every other way of trying to get people to slim down!